Microbial Scl1 Activates TGFBR1 receptor kinase signalling to Drive Fibrosis-Inflammation Axis in Alcohol-Associated Liver Disease
Microbial Scl1 Activates TGFBR1 receptor kinase signalling to Drive Fibrosis-Inflammation Axis in Alcohol-Associated Liver Disease
Yadav, M.; Tripathi, G.; Nandi, A.; Shabnam, S.; Sewak, J. K.; Bindal, V.; Sharma, N.; Yadav, S.; Sharma, V.; Sharma, N.; Mathew, B.; Magar, Y.; Deepanshu, D.; Pandey, S.; Saif, R.; Das, S.; Gupta, A.; Parasar, A.; Sehgal, D.; Sharma, S.; Sarin, S. K.; Maras, J. S.
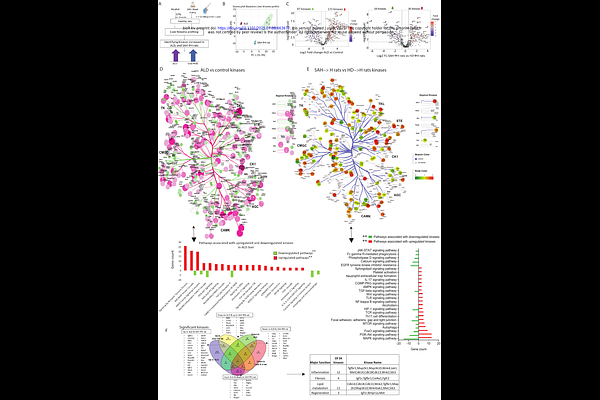
AbstractBackground and Aims: Alcohol consumption alters gut microbiota, which can affect metabolism, immune regulation, and signalling pathways and lead to alcohol-associated liver disease (ALD). We investigated how alcohol-associated gut microbiota (AGMs) modulate liver kinome signalling to drive inflammation and fibrosis in ALD. Method: Liver kinome and metaproteome changes were studied in rats (n=6/group) colonized with stool of severe alcohol-related hepatitis (SAH) patients (SAH to healthy-rats) or healthy human donors (HD to ALD-rats). AGM-associated liver kinome changes were cross-correlated with bacterial genera. A bacterial protein; Streptococcal collagen-like protein 1 (Scl1) was identified with affinity for TGFBR1. This was validated by molecular docking and immunoprecipitation-LCMS assay. Expression of Streptococcus pneumonia and pyogenes was done in stool of SAH patients (n=10). Also, Scl1 was quantified in patient stool (n=24) and liver tissue (n=19) samples. Validation was performed by assessing Scl1 level in plasma and Streptococcus level in stool samples before and after fecal microbiota transplantation (FMT) in SAH patients. Results: Stool metaproteomics showed significant increase in 10 bacterial genera (Streptococcus, Staphylococcus, and Clostridium) in SAH to Healthy-rats, mirroring changes seen in ALD-rats (FC>1.5, p<0.05). Clusters of Orthologous Groups analysis indicated increased post-translational modifications (PTMs) and decreased lipid metabolism in ALD-rats and SAH to Healthy-rats. Liver kinome profiling showed 85 upregulated kinases in SAH to Healthy-rats, with 34 overlapping with ALD-rats, associated with inflammation (Mapk14, Map3k10 and others), fibrosis (Tgfbr1, Igf1r, and others), lipid metabolism (Cdk14, Cdk18) and regeneration (Met, Bmpr1a and others). FMT from healthy human-donors to ALD-rats reversed the expression of Streptococcus (10-fold), Staphylococcus (3-fold), and Clostridium (5-fold), along with 18 kinases associated with inflammation (Btk, Camk4, Nuak1) and fibrosis (Tgfbr1, Col4a1, Fgfr2 and others). Strong association (r2>0.9, p<0.05) was seen between Streptococcus abundance and fibrosis and inflammation-related kinases. Level of Scl1 was significantly high in SAH and ALD-rat stool samples (FC>2, p<0.05). It showed strong affinity for TGFBR1, as validated by molecular docking (>86%confidence) and immunoprecipitation assays (>100FC,p<0.05), indicating it as a potential ligand for TGFBR1. Concordantly, expression of Scl1 was highest amongst all the known ligands for TGFBR1 (p<0.05) suggesting Scl1 is a major contributor for TGFBR1 activation and its downstream signalling in these patients. Following fecal microbiota transplantation, expression of Scl1 in plasma and Streptococcus levels in stool were significantly reduced by 2.1-folds and 1.9 folds respectively in SAH patients. Further, Scl1 levels SAH plasma is capable of predicting poor therapeutic response and 30-day mortality with high accuracy (AUC=0.92, cutoff >70 normalized abundance). Conclusion: Alcohol induced gut dysbiosis alters the liver kinome, promoting inflammation, fibrosis, and lipid dysregulation. Streptococcal Scl1 is identified as a bacterial protein mimicking human collagen and capable of activating fibrotic signalling pathway through TGFBR1in liver and is capable of predicting poor response in SAH. FMT from healthy donor restores microbial imbalance and harmful microbial-host interactions.