Caspase-Driven Microvascular Inflammation and Hypoperfusion in Intravascular Hemolysis: Roles of Leukocyte and Endothelial Activation
Caspase-Driven Microvascular Inflammation and Hypoperfusion in Intravascular Hemolysis: Roles of Leukocyte and Endothelial Activation
Brito, P. L.; Gushiken, L. F. S.; Gotardo, E. M. F.; Figueiredo, V.; Leonardo, F. C.; Costa, F. F.; Conran, N.
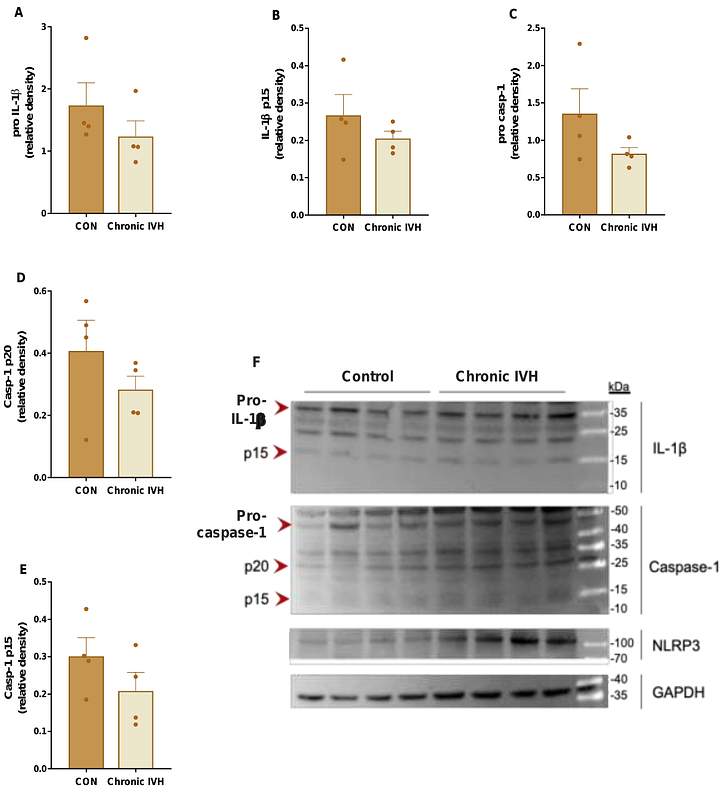
AbstractIntravascular hemolysis (IVH), a pathological process associated with various conditions, triggers vascular responses; however, the molecular and cellular mechanisms driving this process remain unclear. To explore the role of NLRP3 inflammasome- and caspase-dependent pathways in IVH-induced inflammation, we used in vivo models of acute and chronic IVH, alongside heme-stimulation of endothelial cells, thereby isolating this disease mechanism from its etiological causes. Acute IVH induced immediate inflammatory responses in C57BL/6 mice, marked by the release of pro-inflammatory molecules, including IL-1{beta}, within just 15 minutes and NLRP3-dependent caspase activation in circulating leukocytes. Chronic IVH processes in mice elevated liver monocyte-derived macrophage caspase activity and NLRP3 protein expression. In turn, acute IVH impaired cutaneous microvascular blood flow and perfusion, and induced microvascular leukocyte recruitment, which were both caspase-1-dependent. Acute IVH induced time-dependent CD11b-integrin-subunit presentation on leukocytes, while heme stimulation augmented endothelial cell adhesion molecule expression, potentially promoting leukocyte recruitment. This endothelial activation was associated with reactive oxygen species generation, which promoted caspase-1 activation and was key to adhesion molecule upregulation. Our findings highlight a role for inflammasome-/caspase-dependent pathways in hemolytic inflammation, contributing to microvascular leukocyte recruitment and particularly to cutaneous hypoperfusion, a consequence that could facilitate the progression of skin lesions. Targeting caspase-dependent pathways and their downstream effects in disorders that display IVH may offer therapeutic potential for maintaining endothelial integrity, reducing leukocyte activation, and mitigating ischemic injury.